Should IOL reduction be undertaken in higher risk MDS?
- Though patients with int-2/high IPSS risk MDS historically had poor expected OS, therapies such as HMA are now available which improve OS in most subgroups. For patients responding to such agents, IOL reduction should be considered
- For patients achieving TI and a reasonable Hb, serial phlebotomy can be considered, though this has the disadvantage of not suppressing LPI. Consideration should be given to ICT
-
Initial studies indicate good SF reduction and no appreciable increase in AE of DFX:
-
In 40 HR MDS patients treated with DFX outside of clinical trials,
- Median follow-up was 12 months of DFX
- Interruptions for toxicity were seen in 40% and were: GI (n=5, 12.5%) & skin rash (n=4, 10%). 7 (17.5%) had increased serum creatinine >33%, but no progressive increases were seen.
- 4 (3 RA & 1 RAEB-1) had a reduction in transfusion requirement from median 5 to 1 unit/month, with a mean Hb improvement of 2 g/dL (p=0.02)
- The authors concluded that there was no increased toxicity when DFX was used concomitantly with AZA (n=8 int-2 IPSS risk)
-
In 40 HR MDS patients treated with DFX outside of clinical trials,
Higher risk MDS:
-
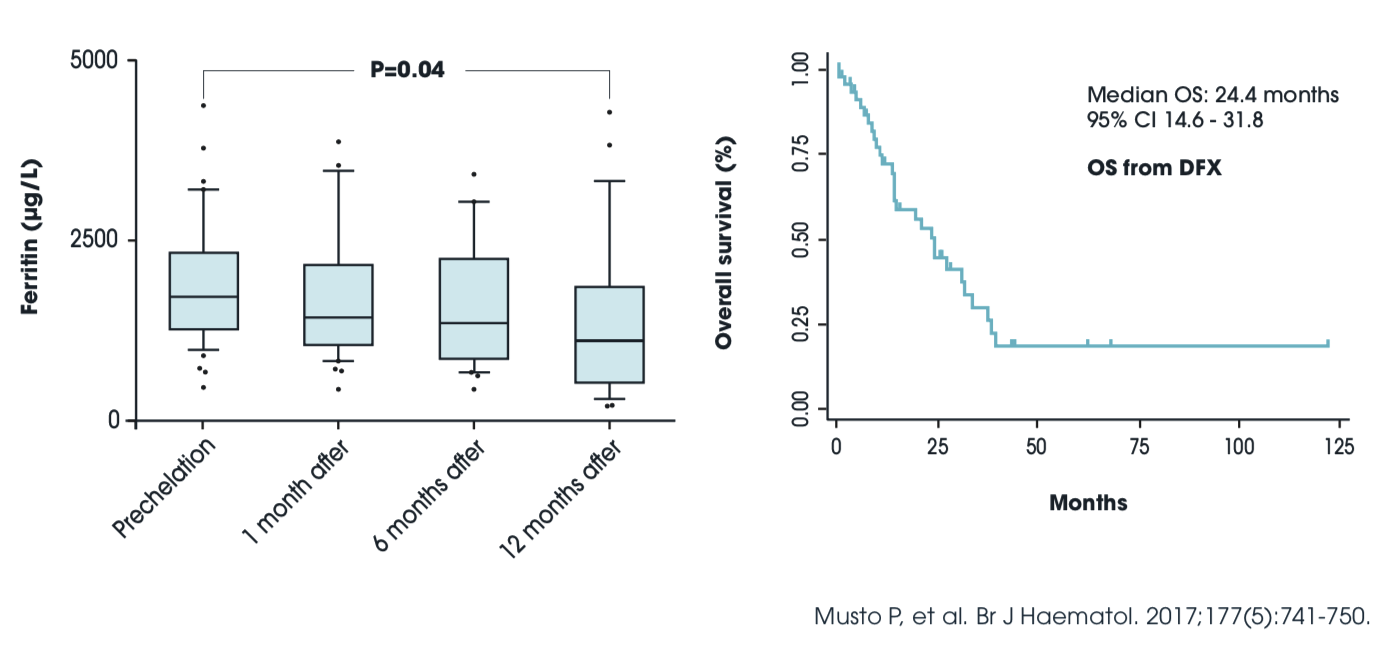
In a retrospective study of 51 intermediate-to-very high IPSS-R risk MDS patients receiving DFX
- 36 (71%) received AZA; 25 received AZA & DFX and 11 received EPO in addition
- Median DFX dose was 1000 (375-2500) mg/day for a median of 11 (0.4-75) months
- 8 (16%) experienced grade 2-3 toxicities (renal or GI), 4 (8%) requiring interruption
- The median SF decreased from 1709 to 1100ng/mL at 12 months (p=0.02)
- During DFX, ≥temporary clinical benefit occurred in 22 patients, and 4 successfully underwent allo-SCT following DFX
- In 1 patient, good HI was observed with DFX treatment only
- Of 17 patients with abnormal transaminases, these improved or normalized on DFX in 8
- The median follow-up was 35.3 months & median OS 37.5 months
- The authors concluded that in HR MDS, DFX was comparable in safety & efficacy to lower-risk MDS & that DFX treatment is feasible and might be considered in selected HR MDS patients